Kneecap dislocations are a common cause of instability and pain in the front of the knee. If left untreated, they can lead to chronic instability and cartilage damage.
Dr. Duff provides expert diagnosis and surgical solutions for kneecap dislocations at his orthopaedic practice.
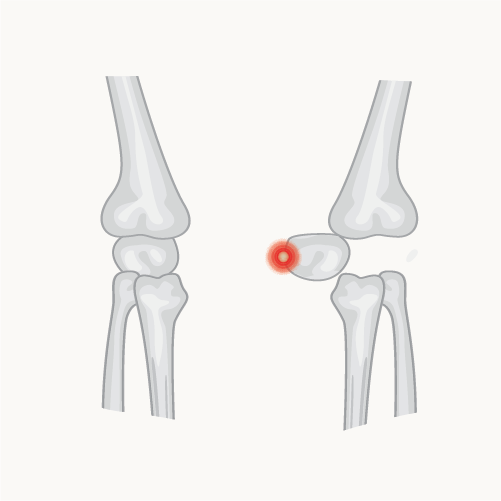
The kneecap (patella) normally sits within a groove at the end of the thigh bone (femur), forming the patellofemoral joint. It is held in place by a combination of bony alignment, ligaments, and balanced muscle forces.
A dislocation occurs when the patella is forced out of this groove, typically toward the outside of the knee. This is often caused by twisting movements or trauma during sports.
Kneecap dislocations can result from an injury, but are more likely if there are anatomical risk factors, such as:
These structural factors can lead to recurring instability after an initial dislocation.
Kneecap dislocations may result from injury or anatomical risk factors like patella alta or hyperlaxity.
First-time cases are often managed with rest and physiotherapy, but surgery may be recommended for recurrent dislocations or if structural issues are present.
If your kneecap dislocates:
For first-time dislocations without fracture, treatment typically includes:
If symptoms improve and the patella remains stable, surgery may not be required.
Surgery is usually advised if:
If you experience significant swelling after a dislocation, a piece of bone or cartilage may have broken off behind the kneecap or in the femoral groove. In this case:
This should be treated as an urgent orthopaedic concern.

Recovery following MPFL reconstruction typically includes:
Dr. Duff will tailor your recovery based on your physical goals and progress in rehab.
If you’ve dislocated your kneecap or are experiencing ongoing knee instability in Australia, Dr. Samuel Duff can provide a detailed assessment and treatment plan tailored to your anatomy and lifestyle.