Significant pain in the groin, deep buttock, side of the hip, or down the front of the thigh, including into the knee.
Hip replacement is a highly successful procedure that relieves pain and restores mobility in patients with advanced arthritis.
Dr. Duff uses a minimally invasive anterior approach to preserve muscle, reduce recovery time, and help you return to everyday activities faster.
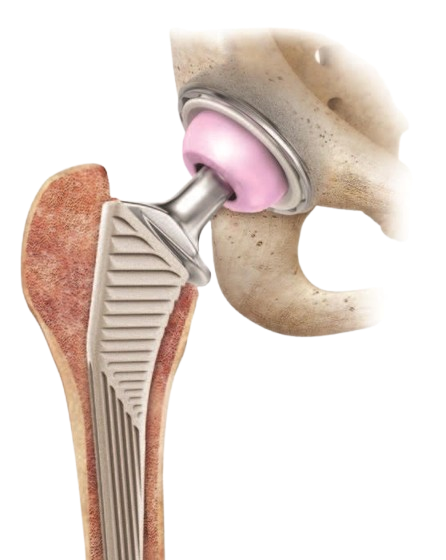
A hip replacement involves replacing the ball and socket of the hip joint with a prosthesis. It is typically made of metal, ceramic, and highly engineered plastic to restore movement and eliminate pain from the hip joint.
Hip replacements are an extremely successful operation and one of the best that modern day medicine offers. You can expect to have an improvement in the range of motion of your hip joint and to have smooth comfortable movement from the articulation.

Dr. Duff offers a direct anterior hip replacement for the vast majority of patients. This approach typically offers:
Initially trained as a physiotherapist, Dr. Duff understands when surgery is or isn’t required and what other treatments are available for your hip condition.
A total hip replacement involved replacing the ball and socket of the hip joint with a combination of titanium, ceramic, and highly engineered plastic. Dr Duff performs this through a minimally invasive muscle sparing direct anterior approach for the majority of patients.
Hip resurfacing involves caping the existing ball and socket joint with a metal-on-metal articulation.
Learn morePartial hip replacements are generally reserved for frail patients who fracture their hip and are not walking significant distances.
Hip replacements are an excellent operation, no matter the approach to perform them. However, an anterior approach offers a minimally invasive, muscle sparing approach to perform a hip replacement.
Patients typically will recover at a faster rate with less pain, a shorter hospital stay and fewer complications, and a less need for walking aids. There are also no restrictions on positions in the postoperative period.
Significant pain in the groin, deep buttock, side of the hip, or down the front of the thigh, including into the knee.
Stiffness, which may manifest as having difficulty touching your foot or being able to place shoes on.
Patients may also find they have a significant problem with walking due to stiffness and pain.
During your consultation, Dr. Duff will assess your symptoms, review your medical history,
and discuss the most suitable options for your hip health.
Undergoing hip replacement surgery is a significant step toward restoring mobility and improving quality of life. While the procedure itself is highly effective, proper preparation is key to ensuring a smooth recovery.
We cover the steps patients should take before surgery, including medical evaluations, physical conditioning, and consultations with healthcare professionals. By understanding what to expect, patients can approach their surgery with confidence and peace of mind.
A hip replacement is a major operation, but often has a relatively easy recovery period. Nevertheless, patients should be in optimum health to undergo the procedure. It’s important that any medical conditions are in good control and that you can optimise your physical health as much as possible with an arthritic hip joint.
Patients will have a consultation with Dr. Duff and also our in-house physiotherapist. A physiotherapist or nurse will help prepare you and your environment to recover well after the hip replacement. We’ll undertake a series of blood tests, imaging of the hip, and some investigations of your heart function to make sure that you are healthy to undergo the procedure. All patients will have careful digital planning of their hip replacement virtually before any surgery.
On the day of surgery, patients will be admitted to hospital after a period of fasting. They should really pay attention to the quality and integrity of their skin in the weeks leading up to surgery. Try to stay off very strong painkillers and keep yourself physically active to be in the optimum state to undergo the procedure.

Patients typically stay one to two nights after their hip replacement. The spinal anaesthetic lasts approximately two hours, and patients are standing on the day of surgery and taking their first steps. The hip is strong and ready to take the full weight of the patient immediately after the surgery.
The next day, patients will undergo an X-ray of the hip replacement and blood tests to ensure they are in good health. They’ll be visited by a physiotherapist to help get you back on your feet and use the new hip replacement.
Emphasise the importance of rehabilitation and the role of physiotherapy in recovery.
The most important principle in the first two to four weeks after your hip replacement is to let the muscles around the hip replacement and all the soft tissues recover from the surgery. This involves not vigorously exercising the hip joint and applying ice packs at regular intervals, and the use of anti-inflammatory medications.
It’s important not to get carried away in the early stages of the rehab to allow these soft tissues to settle. You will benefit with less pain and less swelling by following this approach. Having you ready from four weeks onwards to start strengthening the muscles of the hip joint and getting you back into normal function. The muscles around the hip have had a hard time pulling the stiff bearing that’s been arthritic through its normal range. And so, we’ll need to be strengthened and retrained after the hip has been replaced.
Typically, patients return to driving between 2 and 6 weeks after their procedure, depending on their speed of recovery. They generally walk with an aid for 2 to 4 weeks and have no restrictions on positioning the leg or in any sleeping positions after surgery. Hydrotherapy can begin two weeks after the surgery and offers a very gentle way to reintroduce movement and strength.
There are commercially available cooling machines to help settle the inflammation and pain after surgery. Patients typically need to take some form of stronger painkiller for up to 10 days after the procedure. But it is rare to be on stronger medication longer than this.
A hip replacement is a major operation and comes with some uncommon, but important risks to consider. These risks include infection, blood clots, and fracture of the bones around the hip. Change in leg length and nerve, vessel, or tendon injury are also possible. Tendon injury or the new hip dislocating are additional risks. Thankfully, these complications are very rare.

Dr. Duff takes these important steps to minimise risks:
Modern day hip replacements are successful and long-lasting. Hip replacements have over a 90% survival rate at 20 years in Australia, and are carefully followed up by the national Australian joint registry. At six months after the hip replacement, 96% of patients will say they have better function than before their procedure.
It is one of the most successful operations we have in medicine.
Prosthesis longevity is carefully monitored by the Australian Orthopaedic Association National Joint Replacement Registry. Technology continues to improve, as do the techniques to implant hip replacements.
Based on hips implanted 20 years ago, the survival rate is over 90% for all comers, and expected to improve as our modern day hip replacements approach this timeframe.
After your procedure, you will see the team at Dr. Duff’s office at two and six weeks after the operation. Most patients then don’t need to be seen until one year, but will have physiotherapy to strengthen the muscles around the hip and restore normal walking and movement.
An X-ray will be performed at one year after the procedure to ensure everything is progressing as expected. Dr. Duff will see you at any stage should you have any concerns or need input at other times.

Ready to take the next step? Schedule a consultation with Dr. Duff to discuss your condition, explore treatment options, and get expert guidance on your hip health.
Start your journey toward improved mobility.